Annals of Medical & Surgical Case Reports
(ISSN: 2652-4414)
Research Article
Correlation and Reliability of the Atlas Position on X-Ray in Subjects with and without Cervicogenic Headache: A Retrospective Study
Sillevis R*, Shamus E, Regalado P, Lehigh A
Department of Rehabilitation Sciences, Florida Gulf Coast University, Fort Myers, Florida, USA
*Corresponding author: Rob Sillevis, Department of Rehabilitation Sciences, Florida Gulf Coast University, 10501 FGCU Boulevard south, Marieb Hall 428, Fort Myers, Florida, USA.
Citation: Sillevis R, Shamus E, Regalado P, Lehigh A (2021) Correlation and Reliability of the Atlas Position on X-Ray in Subjects with and without Cervicogenic Headache: A Retroactive Study. Ann Med &Surg Case Rep: AMSCR-100099. DOI:10.53634/2652- 4414.100099
Received date: 06 August, 2021; Accepted date: 20 August, 2021; Published date: 26 August, 2021
Abstract
Background: The exact mechanism causing the development of cervicogenic headaches remains unclear. However, it appears to be the result of dysfunction in the soft tissues, bones, joints, and discs of the upper cervical spine. The position of atlas might correlate with cervicogenic headache. There is no reliable data regarding the inter-and intra-rater reliability when assessing the position of atlas on X-ray. The aim of this study was to evaluate the reliability of identifying a positional default of atlas and the correlation with the presence of cervicogenic headaches.
Methods: Retrospective review of open mouth, lateral, and anterior-posterior X-ray images of 40 subjects with neck pain/ cervicogenic headaches and 41 subjects with neck pain/no headaches. Images were evaluated by double-blinded raters for atlas position.
Outcomes: A good level of reliability was found between raters when identifying atlas position. The average measure of ICC was 0.671 (p<0.01). When determining the level of agreement between the two experienced raters an excellent level of agreement was found. The ICC improved to 0.916 (p<0.01). The lambda statistic evaluating if a non-neutral atlas position was correlated to headaches was significant (p=0.02) with a value of 0.42 indicating a strong relationship.
Discussion: The open mouth view, lateral view and AP view radiographs can be used to reliably evaluate the position of atlas. There was excellent inter- and intra-rater agreement between two experienced clinicians when determining the position of atlas and good inter-and intra-rater agreement when a novice Doctor of Physical Therapy student was included as a rater. Cervicogenic headaches was significantly correlation with a non-neutral atlas position. Further research is necessary to prospectively evaluate the relationship and clinical relevance of the position of atlas and the possible causative relationship of cervicogenic headaches.
Keywords: Atlas positional fault; Cervicogenic headache; Intra-examiner reliability; Inter-examiner reliability; radiograph
Introduction
Around 4% of the population experiences cervicogenic headaches (CGH) [1,2]. The prevalence of CGH ranges from 15% to 20% of all headaches. [3] The International Headache Society defines CGH as “headache caused by a disorder of the cervical spine and its component bony, disc and/or soft tissue elements, usually but not invariably accompanied by neck pain’’ [4].” The exact mechanism causing the development of CGH remains unclear; However, it appears to be the result of dysfunction in the upper cervical spine [1,5,6]. Movement of the upper cervical spine is dependent on stabilizing ligaments, muscles, and the uniqueness of the joint surfaces. The position of the atlas and the mobility of the atlanto-axial (AA) joint appears to correlate with the presence of CGH [7,8]. The stabilizing ligaments maintain the static position of the atlas within the AA and the atlanto-occipital (AO) joints. The transverse ligament stabilizes the atlas to the odontoid process preventing anterior translation of the atlas. The transverse ligament has been identified to be the strongest ligament in the region, and it forms the horizontal fibers of the cruciform ligament connecting the body of the axis to the occiput [9]. Based on the ligament’s position it allows the atlas to move in the transverse plane around the odontoid process. The relatively weaker anterior and posterior joint capsules of the AA and AO joints do not prevent this motion. The only other stabilizing ligament of the atlas is the accessory atlanto-axial ligament. This ligament inserts medially onto the axis’ dorsal surface and spans laterally and superiorly to insert on the lateral mass of the atlas. Based on the fiber orientation, it appears that this accessory atlanto-axial ligament might limit rotation of the atlas on the axis. Despite the stabilizing ligament, the atlas can rotate about 40-45 degrees in the AA joint and contribute more than 50% of the total rotation of the cervical spine [10].
The suboccipital muscles control the movement of the atlas in both the AA and AO. The rectus capitis posterior minor, the obliquus capitis superior, and the obliquus capitis inferior have a direct controlling function of the atlas’ movement in the AA and AO joints and, thus, the position of the head on the neck [11]. Contraction of the ipsilateral obliquus capitis inferior and superior muscles will result in rotation of the atlas. The presence of a “myodural bridge” between the suboccipital muscles and the dura has been previously demonstrated, and this collagenous tissue connection could result in pulling on the dura and, thus, create neural tension of the C2 spinal nerve [12-14]. The significance of the “myodural bridge” might explain the clinical phenomenon of neurotension often identified by clinicians when treating patients with headaches [15-17]. It has been previously proposed that unilateral muscle hypertonicity could result in a positional default of the atlas in the transverse and sagittal planes, and this rotational position of the atlas might be related to the development and maintenance of CGH [7,18,19].
Radiological imaging of the cervical spine has been identified as beneficial to measure postural abnormalities and can be used to obtain an impression about the position and relationship of the upper cervical segments. Standard cervical imaging typically will include three views. The lateral view (LV) can be used to identify the position of the atlas in the sagittal plane. In this view, both the position of the atlas relative to the occiput and the axis can be evaluated, and the position of the atlas itself can be analyzed. If the atlas is in a rotated position, the posterior arches of the atlas likely will not superimpose. Additionally, in this view, an overall impression of the cervical lordosis can be obtained [20]. The open mouth view (OMV) will reveal the position of the atlas relative to the axis. This anterior to posterior view will allow for identifying the spacing between the odontoid of the axis and the lateral mass of the atlas. The unequal spacing could be an indication of a rotatory positional default of the atlas (Figure 1) [21-23]. The third and final view is the anterior posterior view (APV) of the cervical spine allowing for assessing the vertical position of the cervical spine.
While radiological imaging of the cervical spine is considered reliable and valid to evaluate the cervical spine, no data were found regarding the inter-and intra-rater reliability when assessing purely for the position of the atlas relative to the axis using cervical radiographs. The primary aim of this study was to investigate if there is a correlation between the position of the atlas and the presence of neck pain and cervicogenic headaches compared to a control group of neck pain and no headaches. The secondary aim of this study was to evaluate the reliability of identifying a positional default of the atlas.
Methods
This study was reviewed by Florida Gulf Coast University’s Institutional Review Board (IRB) approval before data collection. Based on the fact that this was a retrospective study, and no identifiable subject data were collected, this study was given an “exempt status not requiring IRB approval”. Radiological images of 81 patients (40 with reports of neck pain with cervicogenic headaches and 41 with reports of neck pain without headaches) were collected retrospectively, by a staff member not part of the research team, from the database of a chiropractic office. G*power, version 3.1, was used to perform a priori power analysis with a power of 0.80 and an alpha of 0.05 to detect the ICC and intra-rater reliability. The minimum required subjects were
34 per group. The subject population included those seeking chiropractic care for neck pain with or without headaches. The
pathoanatomical treatment diagnosis and reason for seeking care were not considered in this study. However, the chiropractic physician diagnosed subjects with cervicogenic headaches based on the subject’s history of unilateral headaches preceded by neck pain and a physical examination in which limited active range of motion was identified. The reliability of using these criteria has previously been demonstrated [24]. It was not the intention of this study for the raters to develop or confirm the CGH diagnosis based on imaging. The imaging was only used to evaluate the position of atlas relatively to axis in the study population. The protocol for obtaining the radiological images was the same for all subjects. All radiographs were taken with the subject standing and were obtained by the same chiropractic physician. He has used imaging in his practice for years and uses a standardized approach to obtain these images. Only those subjects were included if three different radiological views, including the open mouth view, were electronically available in the patient’s electronic medical record. All other subjects were excluded.
A copy of the images was collected and de-identified by a staff member, placed in an electronic file and assigned a random subject number. Subjects were all between the ages of 18 to 65. Subject’s age and gender were not collected and were not part of the analysis of data. The collected radiographical images minimally included: anteroposterior open mouth view, lateral view, and anteroposterior view. Figures1, 2, and 3 are examples of the images used in this study. In order to evaluate the intra-rater reliability of each rater, each subject file was duplicated, assigned a subject number, and mixed in the images file randomly. This duplication resulted in 162 subject files for interpretation. This methodology was used so both the inter-rater and intra-rater reliability could be assessed.
The assessment of the images to determine the position of the atlas relative to the axis was performed by one experienced chiropractic physician, one experienced physical therapist, and one doctor of physical therapy student. The chiropractic physician had 14 years of experience managing patients with cervical-related dysfunction. The physical therapist had 26 years of experience managing patients with cervical-related dysfunction. By nature of this study design, the interpreters were blinded to the condition and or history of the patient and the other raters’ rating. Prior to the study initiation, the clinicians discussed how they would assess and determine the atlas’ position using the images. The consensus was to measure the distance between the lateral mass of the atlas and the dens (red lines in Figure 1). This measurement to determine the presence of asymmetry as an indicator for the presence of a rotation of atlas has previously been used and reported [22,25- 27]. The lateral view was used to identify and confirm the atlas’ position based on the visualization of the posterior arch of the atlas and if this was superimposed or not (Figure 2).
Each examiner filled out a datasheet that included the subject number (1-162). On the data sheet, examiners identified if the atlas was in a neutral, right rotated, or left rotated position. This position was determined by measuring the odontoid lateral mass interspace (OLMI) using a simple measuring ruler. Sutherland et al [27] identified that if the right OLMI was smaller than the left side, this indicates a right rotation position of atlas. If the left OLMI is narrower, this implies a left rotation position of atlas. The examiners were instructed to review the subject images to determine atlas position and mark this on a data sheet. The examiners had three weeks to complete the interpretations and were blinded to duplicated images. After the interpretation of all subject files was completed, the three data sheets were provided to a research member who was blinded to which rater created the data sheets and to which subjects were included in this study. In
order to perform the statistical analysis, the ordinal subject data was obtained by using a “1” for a neutral atlas position, a “2” for right rotation of atlas and a ”3” for left rotation. Considering the aim of this study the quantification of the rotation in degrees was not included in the data collection. The research member was also provided with the duplication key for each subject and, thus created a table that included the interpretation of the images of the three raters and the interpretation of the duplicate images. This method allowed for the statistical analysis of intra- and inter-rater reliability and allowed for the blinding of all examiners involved in the image interpretation for this study.
Statistical Analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS), version 26.0, a statistical software package from IBM. All data were analyzed using a confidence interval of 95% and a significance level of 0.05. To correlate the position of the atlas (per agreement of the chiropractor and physical therapist) to the presence of CGH, the Lambda statistic was used (a correlation of two nominal variables). Values between 0 to 0.2 represent a weak correlation, values between 0.21 and 0.4 represent a moderate relationship, and values > 0.41 represent a strong relationship between variables.
The intra-rater and inter-rater reliability to identify the atlas position was calculated using the Intraclass Correlation Coefficient (ICC) (two-way mixed model, single rater). ICC values below 0.40 indicate poor reliability, and fair reliability is achieved with values between 0.41 and 0.59. ICC values between 0.60 and 0.74 indicate good reliability, and excellent reliability is achieved with values greater than 0.75 [28].
Results
Atlas position and cervicogenic headaches
To relate the position of the atlas (neutral, right rotated, or left rotated) to those subjects presenting with a complaint of neck pain with headaches, the Lambda statistics were used. The Lambda statistic is a measure of the association of nominal variables. To identify the number of subjects presenting with a rotated atlas, only those subjects were included in which there was 100% agreement between the chiropractic physician and physical therapist that the subjects presented with a rotated atlas. There was agreement in 33 subjects in which the 20 had a rotated atlas. The lambda statistic evaluating if the rotation of the atlas was correlated to the complaint of headaches was significant (p=0.02) with a value of 0.42, indicating a strong relationship.
Inter-rater reliability interpreting the position of the atlas in radiographs
To determine the inter-rater reliability of all three raters, the ICC was determined. In 9 subjects, one or more raters could not read all radiographs due to clarity issues, thus leaving a total number of subjects to 72 and images reviewed as 144. A good level of reliability was found between raters. The average measure of the ICC was 0.671 with a 95% confidence interval from 0.442 to 0.802 (F (71, 142) = 3.836, p<0.01). When determining the level of agreement between the two experienced raters, an excellent level of agreement was found. The average measure of the ICC improved to 0.916 with a 95% confidence interval from 0.867 to 0.948 (F (71, 71) = 12.079, p<0.01) (Table 1).
Intra-rater reliability interpreting the position of atlas in radiograph
To determine the intra-rater reliability of all three raters between the two sets of images for all subjects, the individual ICC was determined. Rater 1 excluded 11 subjects due to the poor quality of the images preventing proper assessment. The intra-rater reliability of rater 1 was excellent with the average ICC being 0.995 with a 95% confidence interval from 0.992 to 0.997 (F (69, 69) = 189.989, p<0.01). Rater 2 did not exclude any subject’s images from interpretation. The intra-rater reliability of rater 2 was good, with the average ICC being 0.681, with a 95% confidence interval from 0.503 to 0.795 (F (80, 80) = 3.109, p<0.01). Rater 3 excluded 7 subjects due to the poor quality of the images preventing proper assessment. The intra-rater reliability of rater 3 was excellent, with an average ICC of 1.0 (Table 2).
Discussion
The primary aim of this study was to investigate if there is a correlation between the position of the atlas and the presence of neck pain and CGH compared to a control group of neck pain patients with no headaches. Although the true causative factor of CGH remains elusive, it appears that upper cervical spine dysfunction results in the development of cervicogenic headaches. There is a direct neurogenic relationship between the spinal nerves C1-C3 and the trigeminal nerve at the trigeminocervical nucleus [29,30]. In this nucleus, nociceptive afferent input from the upper cervical segments will converge with the trigeminal second-order neuron. This convergence could result in sensitization of the trigeminal nerve and might contribute to the development of CGH. Mulligan described an altered position between bone structures as a “positional fault” [31]. An atlas rotational positional fault resulting from obliquus capitis inferior muscle tonicity would lead to movement restrictions and or pain with movement and could cause nociceptive afferent input and, therefore, contribute to the development of CEG [6,31]. Additionally, connections between the suboccipital muscles and the dura have been identified [13]. These myodural bridges between the obliquus capitis inferior muscles and the dura could lead to unilateral mechanical compression of the C2 nerve root, which might be a contributing factor for the development of CGH [13,32,33]. Increased muscle tone in the suboccipital muscles and the presence of myofascial tripper points in subjects with headaches have been previously demonstrated [34]. The results of this study identify that there is a significant correlation between the presence of a rotatory default position of atlas and subjects with neck pain and headaches. This finding supports the notion that the position of the atlas is a contributing factor to CGH. This finding concurs with a previous report by Sillevis and Swanick who identified a positional default of the atlas in a subject with CGH using musculoskeletal ultrasound imaging.
This study’s secondary aim was to evaluate the inter-rater and intra-rater reliability of novice and experienced clinicians in identifying the position of the atlas. The upper cervical spine is a complex structural anatomy that includes the occiput, atlas, and axis. The motion between the atlas, the axis, and the occiput during head and cervical motions depends on the suboccipital muscles as part of the upper cervical spine’s complex movement control mechanism. This motion is governed by the articular structures' orientation and shape and the strong transverse ligament allowing the atlas to rotate around the dens freely. This rotation of the atlas relative to the axis is the result of the unilateral contraction of the obliquus capitis inferior muscle. It has been previously postulated that unilaterally increased tone in the obliquus capitis inferior muscle due to cervical dysfunction would lead to a relatively rotated position of the atlas on the axis. Despite the fact that there are many types of imaging modalities used to evaluate the anatomy of the upper cervical spine the radiographs remain the golden standard for determining the normal position, alignment, and functioning [35,36].
In this retrospective study, three basic radiographic views of the upper cervical spine were analyzed by three raters. The open mouth view was used to reveal the position of the atlas relative to the axis. This view allows for the identification of the spacing between the odontoid of the axis and the lateral mass of the atlas. (Sutherland et al. 1995) Unequal spacing could be an indication of a rotatory positional default of the atlas. In this view, the position of the spinous process of the axis relative to the dens can be evaluated. The lateral view was used to identify the position of the atlas in the sagittal plane. Singhatanadgige et al [37] demonstrated excellent intra-rater reliability assessing cervical sagittal alignment with ICC ranging from 0.799 to 0.994. The third and final view is the anterior posterior view (APV) of the cervical spine allowing for assessing the vertical positioning of the cervical spine. When using these three views, our study results indicate that our two experienced observers had excellent inter-rater agreement when determining the position of the atlas in the upper cervical spine with an ICC of 0.916 (range from 0.867 to 0.948). Lin et al [38] reported a similar inter-rater agreement when assessing the atlas- lateral mass distance to identify the transverse ligament’s integrity. They identified an inter-rater ICC of 0.983. The intra- rater reliability of our experienced raters was respectively 0.995 and 1.0, indicating excellent intra-rater reliability. These findings were similar to the ICC range of 0.858- 0.968, reported by Lin et al [38]. Our third rater had just completed her first imaging course as a doctor of physical therapy student. Despite this, the ICC of agreement regarding the atlas position between all three raters was good with a value of 0.671 (0.442 to 0.802). This finding implies that after an introductory imaging course, doctor of physical therapy students can determine the position of the atlas in the suboccipital region. Additionally, there was a good level of intra-rater reliability in the third novice rater with an ICC of 0.681 (0.503 to 0.795). Based on this study’s results, the position of the atlas can be reliably identified using three basic radiographic views (OMV, LV, and APV).
Limitations
First, this is a retrospective study; therefore, we relied on the treating clinician’s diagnosis and standardization and radiological imaging protocol. There can be no guarantees that variation in the subject positioning during imaging might alter the spine position which could not be controlled. Standardization of imaging should be used in future prospective studies evaluating the positional relationship between the upper cervical spine and CGH. Secondly, the number of subjects is relatively low (n=81), and the selection of subjects was based on the diagnosis the treating clinician used in his electronic medical records. The diagnoses used to search
this database were neck pain without headaches and neck pain with headaches. It is possible that those subjects presenting with neck pain only could have upper cervical dysfunction, which could have impacted the correlational finding between the atlas position and CGH. Future studies should consider and control for the fact that atlanto-axial dysfunction could be present without headaches. Thirdly, when evaluating the correlation between the atlas position and CGH, only those subjects in which both the experienced raters agreed on the atlas position were included. Based on this, it is possible that there were subjects with a rotated atlas that were not included in the data analysis. Fourthly, based on the fact that the researchers only evaluated the images provided on each subject, they were not able to determine the presence of other musculoskeletal conditions and abnormal postures (such as the forward head position) that could have led to abnormal muscle tone in the upper cervical spine and thus directly affect the atlas position.
Furthermore finally, it is important to point out that the result of this study cannot be used to determine a cause-and- effect relationship between the position of the atlas and the development of CGH. Future studies should further evaluate this possible cause and effect relationship. There remains limited evidence that identifies the clinical utility of cervical radiographs to support clinical-decision making when managing subjects with cervical dysfunction. Despite this lack of evidence, many clinical providers, including the International Chiropractic Association, promote obtaining routine cervical plain films to justify and or determine a therapeutical effect [36]. Radiographs offer a relatively inexpensive imaging option that allows for direct assessment of position and alignment of structures; however, one must consider the potential risk of ionizing caused by the X-ray exposure. For that reason, future research should evaluate if other assessments such as palpation for the atlas position and/or the use of musculoskeletal imaging results in similarly reliable outcomes compared to radiological imaging.
Conclusion
This study demonstrates that there appears to be a strong relationship between the non-neutral position of the atlas and the presence of cervicogenic headaches. The open mouth view, lateral view, and AP view radiographs can be used to evaluate the positional relationship between the atlas and the axis. There was excellent inter-and intra-rater agreement between two experienced clinicians when determining the position of the atlas and good inter- and intra-rater agreement when a novice doctor of physical therapy student was included as a rater. Further research is necessary to prospectively evaluate the relationship and clinical relevance of the position of the atlas and the possible causative relationship of this on the development of CGH.
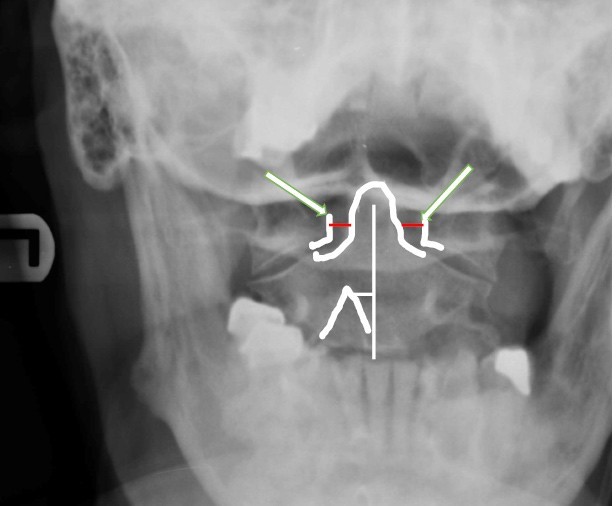
Figure 1: Open mouth view. White Arrows identify the unequal distance between the dens (outlined) and the lateral mass of atlas (outlines). The white line indicates the fact that the spinous process of C2 (outlined as white caret) is not aligned with the dens of C2 in this frontal plane view. The red lines indicate the distance between the lateral border of atlas and the lateral mass of atlas
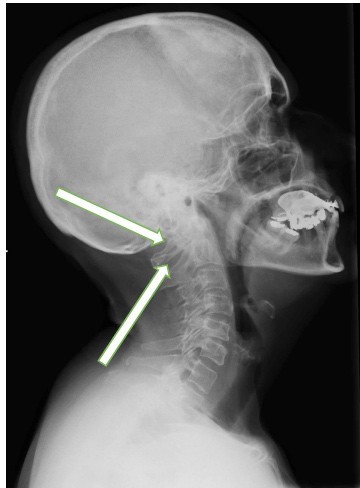
Figure 2: Lateral view C-spine. Arrow indicates that the bilateral arches of atlas (not superimposed) are visual. This view could indicate a relative rotated position of atlas
Figure 3: Anterior posterior view C-spine
|
Intraclass Correlation Coefficient |
||||||
|
|
Intraclass Correlation |
95% Confidence Interval |
||||
|
Lower Bound |
Upper Bound |
Value |
df1 |
Sig |
||
|
All 3 raters |
0.625 |
0.391 |
0.769 |
3.264 |
69 |
<.001 |
|
Experienced 2 raters |
0.901 |
0.842 |
0.939 |
10.202 |
69 |
<.001 |
Table 1: Inter-rater ICC value
|
Intraclass Correlation Coefficient |
||||||
|
|
Intraclass Correlation |
95% Confidence Interval |
||||
|
Lower Bound |
Upper Bound |
Value |
df1 |
Sig |
||
|
Rater 1 |
0.995 |
0.992 |
0.997 |
189.986 |
69 |
<.001 |
|
Rater 2 |
0.681 |
0.503 |
0.795 |
3.109 |
80 |
<.001 |
|
Rater 3 |
1 |
. |
. |
. |
73 |
0 |
Table 2: Intra-rater reliability
Citation: Sillevis R, Shamus E, Regalado P, Lehigh A (2021) Correlation and Reliability of the Atlas Position on X-Ray in Subjects with and without Cervicogenic Headache: A Retroactive Study. Ann Med &Surg Case Rep: AMSCR-100099. DOI:10.53634/2652- 4414.100099